Abstract
The co-occurrence of myeloproliferative (MPN) and lymphoproliferative neoplasms (LPN) is rare and many publications have been limited to small case reports. Others have involved a considerable number of patients, but the coexistence remains underreported and inadequately studied. A recent retrospective review reported that a MPN patients have a 2.8-fold higher relative risk of developing LPN.
A database developed at Weill Cornell Medicine (WCM) was queried for patients with ≥3 visits between 1998-2018 with a diagnostic code for a MPN and lymphoma or myeloma subtype. Patients identified were verified to ensure that study inclusion criteria were satisfied. Observed co-occurrence was compared to nation-wide reported prevalence.
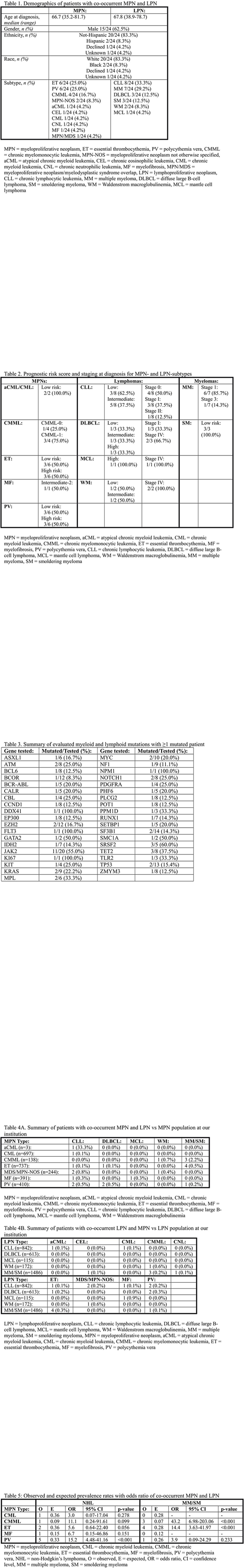
Demographic and clinical details of 24 patients with a MPN and LPN were recorded (Table 1). The ratio of males to females was 1.7. Essential thrombocythemia and polycythemia vera, and chronic lymphocytic leukemia (CLL) were the leading MPN and LPN subtypes, respectively. Patients were assigned to risk or staging categories at diagnosis based on subtype-specific criteria (Table 2).
Median values for diagnostic bone marrow biopsy findings in 14 patients were 2% [0-5] for myeloblasts and 80% [15-100] for cellularity. Additionally, 10 patients had evaluated reticulin fibrosis: 5 (50.0%) presented as MF-0, 4 (40.0%) as MF-1, and 1 (10.0%) as MF-2.
Progression to myelofibrosis was confirmed by morphology in 1 (4.2%) patient 10.1 years after a polycythemia vera diagnosis and 5.4 years after a diffuse large B-cell lymphoma (DLBCL) diagnosis. Progression to acute myeloid leukemia was confirmed by morphology in 1 (4.2%) patient 2.4 years after a chronic myelomonocytic leukemia diagnosis and 1.2 years after a smoldering myeloma (SM) diagnosis.
Interphase fluorescence in situ hybridization (iFISH) detected cytogenetic abnormalities in 5/8 (62.5%) CLL patients: 2/5 (40.0%) and 5/5 (100.0%) patients harbored deletions in trisomy 12 and 13q14, respectively. Immunoglobulin heavy chain variable region gene (IGVH) status was unmutated in 2 (25.0%) patients. One (12.5%) patient was CD38+ and 2/6 (33.0%) patients were ZAP-70+. At diagnosis, all 8 patients presented with early stage disease (Rai stage 0-II). Based on the CLL-specific international prognostic index (IPI), 3/8 (37.5%) and 5/8 (62.5%) presented as low-risk and intermediate-risk, respectively.
Of the 6 lymphoma patients: 5 (83.0%) patients presented with Ann Arbor stage-IV disease at diagnosis. Four (66.7%) patients presented as low/intermediate-risk, and 2 (33.3%) presented as high-risk based on disease-specific IPIs. One patient presented with -17p by iFISH. All 4 patients that were evaluated for Ki-67 had moderate/high expression.
Of the 7 multiple myeloma (MM) patients, 6 (85.7%) presented as stage 1 and 1 (14.3%) as stage 3. Of the 3 SM patients, all 3 presented as low risk [12]. In addition, these patients were categorized as IgG-K (4; 40.0%), IgG-L (2; 20.0%), IgA-K (1; 10.0%), IgA-L (1; 10.0%), IgM (1; 10.0%), and biclonal IgG-L/IgA-L (1; 10.0%) [13].
Mutation statuses were identified by commercially tested myeloid or lymphoid molecular panels. As expected in this MPN subtype distribution, 11 (45.8%) are JAK2+, 2 (8.3%) are MPL+, 1 (4.2%) is BCR-ABL+, and 1 (4.2%) is CALR+ (Table 3).
The risk of a co-occurrent MPN and LPN is higher than expected if they are mutually exclusive (Table 4A-4B, 5). Of interest, 13 (54.2%) patients were diagnosed with a MPN 11.8±18.8 years prior to a LPN; conversely, 11 (45.9%) were diagnosed with a LPN 6.5±6.2 years prior to a MPN. In addition, MPN therapy was started 2.0±2.3 years after a MPN diagnosis, and LPN therapy was started 2.6±4.0 years after a LPN diagnosis. A review of survival analysis requires larger subtype populations since the degree of survival can vary greatly, but it has been reported that patients with a MPN or LPN have significantly reduced life expectancy when compared to the general population. Median follow-up for our patient is 8.2 years (1.5-28.0) with 17/24 (70.8%) patients still being actively followed at our institution, 6 (25.0%) are been lost to follow-up, and 1 (4.2%) is deceased.
The significant prevalence of these hematologic malignancies in combination emphasizes the importance of performing a bone marrow biopsy, which we espouse at our institution, cytogenetic analysis, and myeloid and lymphoid molecular testing to identify mutations.
Furman:Loxo Oncology: Consultancy; Gilead: Consultancy; Verastem: Consultancy; Acerta: Consultancy, Research Funding; TG Therapeutics: Consultancy; Incyte: Consultancy, Other: DSMB; Pharmacyclics LLC, an AbbVie Company: Consultancy; Genentech: Consultancy; Sunesis: Consultancy; Janssen: Consultancy; AbbVie: Consultancy. Niesvizky:Amgen Inc.: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Celgene: Consultancy, Research Funding; Janssen: Consultancy, Research Funding; Takeda: Consultancy, Research Funding. Ritchie:Bristol-Myers Squibb: Research Funding; Novartis: Consultancy, Other: Travel, Accommodations, Expenses, Research Funding, Speakers Bureau; Astellas Pharma: Research Funding; NS Pharma: Research Funding; Celgene: Consultancy, Other: Travel, Accommodations, Expenses, Speakers Bureau; Pfizer: Consultancy, Research Funding; Incyte: Consultancy, Speakers Bureau; ARIAD Pharmaceuticals: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal